Pain relief after major surgery
This page gives you information about the main pain relief options available after major surgery. You will probably only need this pain relief for the first few days following surgery. Pain is to be expected after surgery and poor pain relief can increase the risk of complications. Our aim is to make sure that you receive the best possible pain relief. Good pain relief is a high priority, the benefits are: • It can help you to get better. • Your overall experience will be much better. • It can shorten the length of your hospital stay. • It can reduce your risk of complications such as developing a chest infection.
Before your operation
Your anaesthetist will visit you before your operation and talk with you about the ways in which your pain can be controlled. The anaesthetist will take your general health and the type of surgery you are having into consideration when making any decisions.
Please tell the medical staff and the anaesthetist if you normally take regular strong pain relief at home, such as morphine or pain relief patches, as adjustments to your pain relief may be necessary. You will normally continue with your usual pain relief (that you take at home) during your hospital stay.
Pain assessment
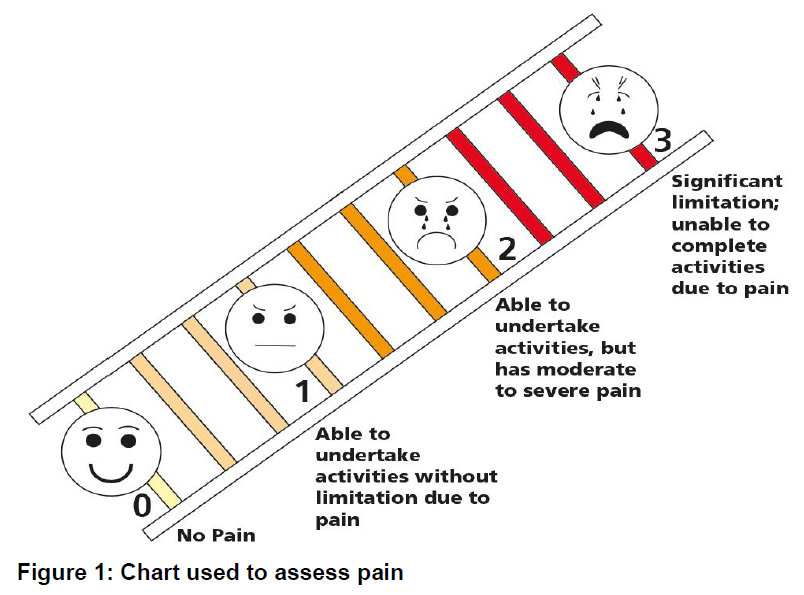
The nursing staff will regularly assess your pain using the pain chart below (see Figure 1).
You must inform nursing staff if you have moderate to severe pain despite having pain relief so that your current pain relief medication can be reviewed. You must be able to deep breathe/cough and move comfortably.
The most common methods of pain relief used at Gloucestershire Hospitals NHS Foundation Trust are:
Patient Controlled Analgesia System (PCAS)
PCAS is an electronic pump, which delivers pain relief through a cannula (a thin tube inserted into a vein in your arm). To receive the pain relief, you simply press the button on the device you are given to hold in your hand, until you hear the pump bleep. This signals the pump to give you a measured amount of pain relief into your vein. You should start to feel more comfortable within a few minutes. This system means that you are in control of your pain relief.
The pump is programmed so that you will not be able to give yourself more than the prescribed dose of pain relief. It will not give you doses of pain relief more often than every 5 minutes. This gives each dose time to work.
You may press the button as many times as you like so that you are comfortable. The hand set should only be pressed by you. Nursing staff will carry out regular checks while you have this method of pain relief.
Epidural infusion
For some operations, such as major abdominal surgery, an epidural can give good pain relief. Only small quantities of the pain relief medication are needed because they act directly on the nerves that carry pain signals to your brain. This type of pain relief means that you should be able to get up and about soon after your operation.
If the anaesthetist thinks an epidural is needed, they will discuss this with you fully so that you understand all of the risks and benefits. The anaesthetist will be happy to answer any questions you may have.
The nerves in your back, pass through an area close to your spine called the epidural space. Either before your surgery, or while you are under the anaesthetic (asleep), the anaesthetist will carefully place a thin plastic tube (catheter) into the epidural space. During the operation the anaesthetist will use this catheter to give pain relief by injecting local anaesthetic into the epidural space. As a result, the nerve messages are blocked so that when you wake up you should feel comfortable. You may notice that your legs and abdomen feel quite numb and heavy. This is normal and will wear off over the next few hours. Sometimes other pain relief medications are given alongside the epidural.
The catheter will be used to give you pain relief (local anaesthetic and fentanyl) continuously during the early part of your recovery period (usually 2 to 3 days).
While the epidural is in place, nursing and medical staff will make regular checks of how well your pain is controlled and if you have any loss of sensation/numbness. They will make any necessary adjustments to the epidural pump to make sure that you are comfortable and safe.
You should be able to breathe deeply and cough comfortably but if you experience pain at those times, please let the nursing staff know.
If you notice an increase in numbness or weakness in your limbs or back pain you should report this to your nurse and doctor straight away.
Occasionally patients with epidurals may experience some itching in the lower abdomen or legs which can be easily treated as soon as you let your nurse know.
Patients with an epidural normally have a tube placed in their bladder to drain away urine; this is known as an indwelling urinary catheter. This is because the epidural can make it difficult to pass urine while it is in place. The urinary catheter is normally removed once the epidural has been taken out.
You may be given a device with a button to press, similar to the PCAS, which is linked to the epidural pump. This means you are able to give yourself additional medication from the device if you need it. This is known as Patient Controlled Epidural Analgesia (PCEA). The pump is programmed and will not allow you to have more than the prescribed dose. This system puts you in control of your pain relief.
You will be reviewed by a member of the pain service or anaesthetic team once a day including the day after the epidural catheter removal.
Local Anaesthetic (LA) infusions
An anaesthetist or surgeon may place one or two catheters (fine tubes) in or near your wound. This is usually attached to a device containing local anaesthetic and will give you a continuous dose into the wound to make you more comfortable. This is normally used alongside other forms of pain relief such as patient controlled analgesia and regular pain medication by mouth.
Rectus sheath catheters
Two fine plastic tubes (catheters) are placed one each side of your six pack muscles, in your abdomen, during your operation. Every 6 hours a measured dose of local anaesthetic (LA) is given through these catheters via an electronic pump by the nurse looking after you.
The catheters usually stay in place for 3 days. Often other forms of pain relief, such as patient controlled analgesia and regular pain medication by mouth are given alongside this method of pain relief.
Spinal anaesthetics
Your anaesthetist may suggest putting some local anaesthetic and opiate, such as morphine, into the lower part of your back before your operation. This blocks the nerves in the lower part of your body to give better pain relief after surgery. The local anaesthetic will give you heavy numb legs for about 2 to 3 hours after the surgery. Depending on the type of surgery you are having you may then be given a general anaesthetic or some sedation before the operation takes place.
Oral pain relief
Nursing staff will regularly assess how comfortable you are and you will receive regular doses of pain relief by mouth. This will normally include paracetamol, ibuprofen (as long as you do not have a history of stomach ulcers, aspirin sensitive asthma or poor kidney function) and codeine or tramadol. Both codeine and tramadol can make you feel light headed, nauseated (feeling sick) or constipated so we only give it to you if your pain is not controlled by paracetamol and /or ibuprofen
If you take codeine or tramadol for a week or more, do not stop these medications suddenly as you may experience some withdrawal symptoms such as shivering. It is better for you to reduce them gradually.
Paracetamol and ibuprofen work in different ways and when taken at the same time as other pain relief medication will improve your overall pain relief. Paracetamol and ibuprofen can reduce the amount of other pain relief medication needed.
If your doctor has prescribed regular pain relief, it is important you take them at the time the nurse offers them to you, even if you are not in pain. This helps to keep your pain under control between doses of pain relief medication.
If you are not allowed to eat or drink following surgery, you may still take these pain relief medicines with a small amount of water (excluding ibuprofen which should always be taken with food).
You must let the nursing staff know if the regular pain relief does not help you to move, breathe deeply or cough comfortably.
The doctor may consider prescribing you additional strong pain relief medication such as liquid morphine or oxycodone., to boost your regular pain relief. These medications may take about 40 minutes to work.
Some pain relief can be given directly into your vein (IV) via a tube called a cannula.
Nausea
You may be worried about the possibility of feeling sick or vomiting after your operation, but you will be prescribed medicines to treat this. There is good evidence to suggest that you are less likely to feel sick if your pain is well controlled.
Pain relief at home
You may be given a supply of pain relief medication to take home. As your body starts to heal your pain will reduce and you will be able to lower the amount of pain relief that you take.
You should take paracetamol regularly while you gradually reduce and stop the other pain relief medications. Sometimes these may contain strong pain relief (opioids) such as tramadol, codeine, morphine or oxycodone which should be stopped first. Opioids need to be reduced gradually and then stopped.
If you have been given ibuprofen, stop this next and paracetamol last.
During this process if you feel that your pain starts to increase, you should increase the pain relief that you have reduced then start to reduce it again after a few days.
If you require more pain relief medication, paracetamol and ibuprofen can be obtained from the supermarket or pharmacy. You will need to contact your GP if you require stronger pain relief.
Your GP may want to speak to you before prescribing more opioid pain relief. It is recommended that people take the lowest dose of opioids for the shortest period of time to avoid harm from long term opioid use for non-cancer pain.
Opioids and driving
Opioid pain medication can affect your ability to drive. Speak to your GP if you are unsure if you should be driving. Further information can be found at: www.gov.uk/drug-driving-law
References
Acute Pain Management: Scientific Evidence: Fourth Edition 2015. Australian and New Zealand College of Anaesthetists.
Analgesic Ladder. World Health Organization; 1986.
Best practice in the management of epidural analgesia in the hospital setting (2010) Faculty of Pain Medicine: The Royal College of Anaesthetists.
Understanding and Managing Pain after surgery. The British Pain Society. Available at:
https://www.britishpainsociety.org/static/uploads/resources/files/Taster_for_web_Aug_2017.pdf
Epidural pain relief after surgery (patient information leaflet) Fifth Edition February 2020. Royal College of Anaesthetists. Available at:
https://www.rcoa.ac.uk/sites/default/files/documents/2020-03/05-EpiduralPainRelief2020web.pdf
Further information
Royal College of Anaesthetists
Website: https://www.rcoa.ac.uk/sites/default/files/documents/2019-10/05-EpiduralPainReliefweb.pdf
The British Pain Society
Website: http://www.britishpainsociety.org.uk/
Drugs and Driving: The Law.
Website: www.gov.uk/drug-driving-law