Endoscopic Ultrasound (EUS)
You have been offered an Endoscopic Ultrasound (EUS) to help us assess or treat your condition. The information on this page will help to answer any questions you may have. It is important that you read this page before coming in for your appointment as it gives you important information about this investigation.
If you are pregnant, taking warfarin, other blood thinning medication or any medications for diabetes please contact the Endoscopy Department as soon as possible for advice. Your test may be delayed if you have not asked for and taken advice.
The length of time you will be in the department will vary but may be anything from 2 to 4 hours. Please ask the nurse admitting you to the department for further information during your admission check.
Please remember that your appointment time is not the time you will have your investigation, this will take place after checks have been carried out and you are ready to have the procedure.
What is EUS?
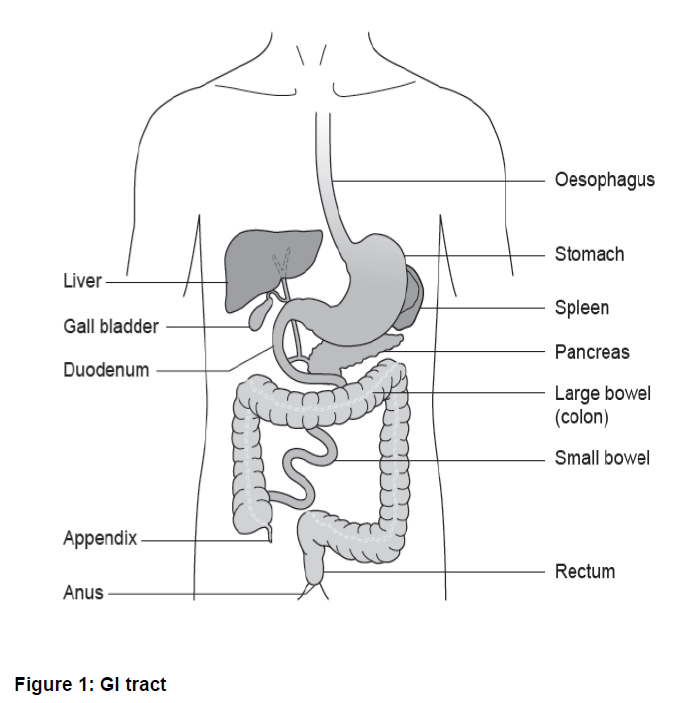
EUS is a specialist procedure that combines the ability to look directly at the linings of the upper gastrointestinal (upper GI) tract with ultrasound. Using ultrasound enables the endoscopist (a doctor specialising in Endoscopy) to see the structures beneath the surface and other organs that are near the upper GI tract including the lungs, liver, gall bladder and pancreas.
Sometimes, during an EUS the endoscopist may take fluid or tissue samples which are sent to the laboratory for examination. EUS may also be used to guide other procedures such as cyst or abscess drainage and in certain conditions is used to guide a special injection as treatment for severe pain; this is called a Coeliac Plexus Neurolysis (CPN).
Why is EUS done?
EUS is a specialist test that gives your doctor detailed images of your digestive tract and the tissues nearby.
EUS is used to get a more detailed picture of known abnormalities, which were found at earlier endoscopy procedures, or were seen on X-ray tests such as Computed Tomography (CT) scans. The information provided by EUS can help guide treatment more accurately.
Alternative treatments
There are no alternative treatments but if you wish to discuss what it would mean if you chose not to have this test, please speak to the doctor who referred you.
Before the procedure
To allow a clear view by the endoscopist, the stomach must be empty, so please follow these instructions:
- Do not have anything to eat for at least 6 hours before the procedure apart from your regular medication with clear fluids such as water
- Do not drink milk for 4 hours before the procedure. This is because milk will line the stomach and not allow a clear view
- You may drink water up to 2 hours before your procedure
On admission
- You will be seen by a nurse who will check your personal details and ask you some questions about previous illnesses, operations and medication. Please bring a list of any medicines you are taking. You will also be asked if you have any allergies or reactions to any medication
- If you wish to have sedation, you will need to arrange for a responsible adult to take you home and to stay with you for 24 hours
- You will be asked to sign a consent form. By signing this form, you will be agreeing to have the test and that you understand why it is needed. This does not take away your right to have the test stopped at any time
For the time that you are in the Endoscopy Department, we want to provide a safe, supportive environment. Please feel free to ask questions if you have any worries or concerns. For this procedure you will not need to remove any clothes, but ties may need to be loosened and shirts opened at the neck.
Sedation and throat spray
A local anaesthetic spray may be used to make the back of your throat numb and more comfortable during the procedure. You will be asked not to have anything to eat and drink for up to 1 hour after the spray is given because it reduces the sensation in your throat and may cause food and drink to go down your windpipe.
Your first drink after the procedure should be cool and sipped slowly. You will usually be given this drink while you are in the recovery area.
A small plastic tube (cannula) will be placed into a vein usually in the back of your hand or into your forearm. This is inserted to give you sedative medications before or during the procedure.
A sedative will make you sleepy and relaxed during the procedure, but not unconscious. This is known as conscious sedation and although drowsy, you will still hear what is said to you and will be able to follow simple instructions during the investigation.
During the procedure
In the procedure room, you will be asked to remove any false teeth and glasses. You will be asked to lay on your left side and will be made as comfortable as possible. A plastic mouth piece will be placed between your teeth and gums to help us guide the endoscope.
Your pulse and oxygen levels will be monitored throughout the procedure and your blood pressure will be taken from time to time. Oxygen will also be given through a small sponge inserted into one of your nostrils.
The endoscope is passed through the mouth guard to the back of your throat. You may be asked to swallow or take a deep breath in at this point to help the tube go down into your oesophagus (food pipe). This does not interfere with your breathing.
The procedure will take up to 30 minutes to complete. During this time some air will be passed down the tube to inflate your stomach and allow the endoscopist a clearer view. You may feel some wind-like discomfort and belch some air during the test but please do not feel embarrassed as this is a common reaction. The air is sucked out at the end of the procedure.
Any saliva in your mouth will be removed by the nurse caring for you using a small suction tube; like the one used at your dental surgery.
Risks associated with having sedation
Sedation can sometimes cause problems with breathing, heart rate and blood pressure. Careful monitoring by a fully trained endoscopy nurse makes sure that any potential problems can be spotted and treated immediately.
Complications
Endoscopic ultrasound procedures carry a very small risk (1 in 10,000 cases) of haemorrhage (bleeding) or perforation (tear) of the gut, which can mean that surgery, may be necessary to repair it. The use of guided needle sampling slightly raises the risk of bleeding, but it is important to state that the risk is very small. The risk of perforation is about 1 in 1,000 cases when using an endoscope to take samples with EUS.
There is a similar risk of causing inflammation of the pancreas (pancreatitis).
Infection is rare but can happen during the removal of fluid from cysts, (known as aspiration), so you may be given antibiotics to reduce the chance of this happening.
If you have had a Coeliac Plexus Neurolysis (CPN), we will monitor your blood pressure for a while after the procedure. CPN may temporarily lower your blood pressure, but this is not common.
Some patients may have diarrhoea for a few days after the procedure due to a temporary effect on the nerves that supply the intestine. A very small number of patients may experience a temporary increase in pain.
As with all endoscopic procedures there may be a slight risk to teeth, crowns or dental bridgework; you should tell the nurses if you have either of these fitted.
Other rare complications include a condition called ‘aspiration pneumonia’, which is inflammation of the lungs caused by breathing-in or choking on vomit, adverse reactions to intravenous sedative medications and, when used, antibiotic treatment.
Like all tests, this procedure will not always show up all abnormalities and, on rare occasions, a significant abnormality may not be seen. If you have any questions about this, please ask either a member of staff at the time of your procedure, or the person who referred you.
After the procedure
The nurse caring for you will take you to the recovery area after the procedure, where observations will continue. This is called the recovery period.
You may feel a little bloated or have some discomfort in your lower abdomen after the test, due to small amounts of medical air being inside you.
After the procedure, you will need to stay in hospital for about 30 to 60 minutes, unless otherwise advised by the clinician. This will also depend on how well you recover from the sedation.
If no sedation has been used you will be allowed to go home after being given your discharge information.
Normally, you do not see the person who carried out the procedure before going home. In most cases the discharging nurse will give you a copy of your endoscopy report and written discharge instructions before you leave.
A side effect of sedation is that you can forget what has been said to you so it is a good idea to have someone with you at this stage.
Discharge home
If you have been given sedation for this procedure, you must arrange for someone to take you home and a responsible adult to stay with you for the following 24 hours. You may go home by taxi but you must have someone with you on the journey.
For this period of time, you should not:
- drive a car, motorbike or ride a bicycle
- drink alcohol
- operate machinery or do anything requiring skill or judgement
- make any important decisions or sign any legally binding documents
Test results
Please contact your GP or consultant directly for your test results as these are not disclosed to Endoscopy.
Follow up
Your doctor will contact you to discuss when you will come back to the clinic.
Contact information
If you have an enquiry about your appointment date or time, please contact the Booking Office.
Booking Office
Tel: 0300 422 6350
Monday to Friday, 8:00am to 4:00pm
Medication Advice Line (answer machine)
If you have any questions relating to your medication, please leave a message and a member of staff will return your call:
Cheltenham General Hospital
Tel: 0300 422 3370
Gloucestershire Royal Hospital
Tel: 0300 422 8232
Other Endoscopy Units
Cirencester Hospital
Tel: 0300 422 6294
Stroud General Hospital
Tel: 0300 421 8073