Enhanced recovery pathway for colorectal surgery
When you are admitted to hospital for your bowel operation you will be taking part in what is called an ‘enhanced recovery pathway’. This programme of care aims to help you recover quickly and safely. During your hospital stay there will be daily recovery goals which you will be encouraged to achieve. A team of doctors, nurses and other healthcare staff will be monitoring your progress and will support you in reaching your goals. The information on this page should help you understand more about the key areas of the pathway, and will tell you how you can play an active part in your recovery. If there is anything you are not sure about, please ask a member of staff involved in your care.
On this page
-
Before you come into hospital
-
Preparation before your surgery
-
After your surgery
-
Staying out of bed and walking
-
Visitors
-
Discharge criteria and arrangements
-
Important discharge information
-
Your wound
-
Your bowels
-
If you have a stoma
-
On the day of your discharge the stoma nurses will give you a supply of equipment, which you will need, to care for your stoma. The stoma nurse responsible for your care will discuss any concerns you may have about the care of your stoma when they contact you. This is usually by telephone. The stoma nurse may arrange to visit you at home or to see you in an outpatient’s clinic. You will be given contact telephone numbers and information and advice relating to your stoma before you are discharged from hospital.
-
Exercise, hobbies and activities
-
Work
-
Many people are able to return to work within 4 to 6 weeks after their surgery. If your job involves heavy manual work then we would advise that you take 6 weeks off.
-
Sex
-
Driving
-
Questions or concerns
-
Contact information
Before you come into hospital
You will be involved in planning your care and recovery from the time that we see you for your pre-admission assessment. This is an opportunity for you to tell us all about your individual needs and circumstances. Please allow a couple of hours for this appointment. You are welcome to bring a family member or companion with you.
If you take any medications (including inhalers) we ask that you bring these along with the medication list provided by your GP to your pre-assessment appointment. Can you also bring a bag as you may be given some drinks to take home with you.
Please start to think about your discharge. It is important that you tell us as early as possible if you have any concerns about whether you will be able to manage your daily activities when you are discharged after your operation.
We have healthcare staff including physiotherapists, occupational therapists, social workers and the discharge assessment team who will be able to arrange any support you might need.
Preparation before your surgery
Admission to hospital
You will either be admitted directly to a colorectal ward, or to a surgical admissions suite (you will then be moved to a colorectal ward for your care after surgery). The colorectal ward at Gloucestershire Royal Hospital is Ward 4A and at Cheltenham General Hospital it is Dixton Ward.
Your consultant will decide, depending on the type of operation, if you need a laxative medication to clear out the contents of your bowel before the surgery:
- You may be admitted to the ward the day before your operation to take a laxative medication. You will have a fluid drip (thin tube) inserted into a vein in your arm. The drip will allow us to replace the fluids and salts in your body which will be lost due to the effects of the laxative.
- You may be asked to take a laxative medication at home to clear out the contents of your bowel. We will give you a leaflet, along with the medication, to explain how and when to take the laxative.
- If you are not asked to take the laxative medication, you may need to have an enema 1 to 2 hours before your operation, to clear the lower end of the bowel. This will be given when you are admitted to the surgical admissions unit.
- Some patients may not need any bowel preparation at all.
PreOp® drinks
As part of the enhanced recovery pathway (ERAS) you will be asked to drink 4 small cartons of a lemon flavoured carbohydrate drink. If you have diabetes, you will not be able to take these drinks as we need to keep your blood sugars stable. These drinks need to be taken before you have your operation as they will give you the extra energy needed to help you recover. You will be given instructions at your pre-admission appointment or from your Colorectal Specialist Nurse about when you need to take them.
If you need a stoma (ileostomy/colostomy)
If you have been told you may require a stoma, you will already have met one of the stoma care nurses. The stoma nurses will support you with your stoma and provide any information needed. They will see you again just before your operation to mark a suitable site on your abdomen for your stoma. While you are in hospital, the stoma care team and the ward nurses will help you with learning to manage your stoma.
After your surgery
Preventing blood clots
While you are in hospital you will be given a daily blood thinning injection called Fragmin®. This helps to reduce the risk of blood clots (thrombosis) forming in the legs and lungs. Some patients will be advised to have a 28 day course of Fragmin® after their operation, in which case you may be taught to self-administer the injections so that you can manage after your discharge from hospital. You will be told at your pre-assessment appointment if this will be the case.
You will also be asked to wear compression stockings to help prevent blood clots from forming.
Eating and drinking
On the day before your surgery, you will be able to eat and drink unless you have been advised to have a ‘low residue’ diet. If you have been asked to take medication to clear the contents of your bowel you can only have clear fluids once you have started the laxative. If this applies to you, it will have been discussed at your pre-admission appointment.
It is important that you eat and drink as soon as possible after your operation. Your body will benefit from taking in nutrition and it will help your overall recovery. You will be given 3 drinks (either juice or milk based) each day to improve your nutrition while you are in hospital.
Sickness
Sometimes after an operation, a person may feel nauseous or be sick. This is usually caused by the anaesthetic or other medications which we use. You will be given medication during surgery to reduce this. If you feel sick following your surgery, please tell a member of staff as they will be able to give you something to relieve it. It is important that we relieve your sickness to allow you to feel well enough to eat and drink normally.
Pain control
Effective pain control is an essential part of your enhanced recovery pathway. This will allow you to deep breathe effectively, start walking around and help you to sleep.
The type of pain relief used will depend on your circumstances and the operation you are having. You will be given a leaflet during your pre-assessment appointment explaining the types of pain control available. The anaesthetist will discuss the options with you before the operation.
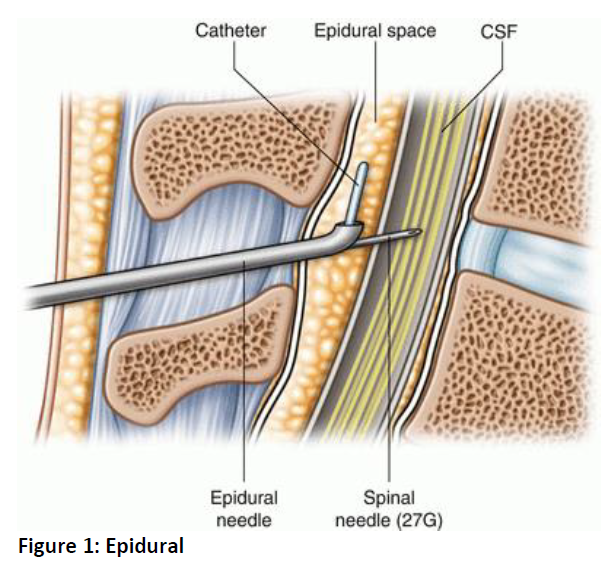
Some patients may be offered an epidural which can stay in for 3 days giving a continuous supply of pain relief via a fine plastic tube inserted in your back. In some cases, a spinal anaesthetic may be more effective and this is given through a single injection in your back.
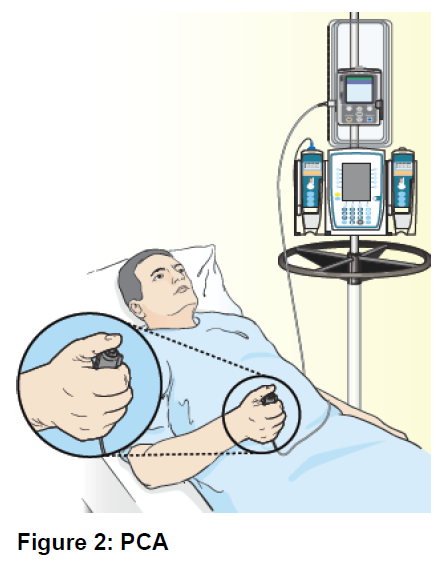
You may also be offered a ‘pain pump’ known as Patient Controlled Analgesia’ (PCA) which allows you to give yourself a small amount of pain relieving medication (usually morphine) when you need it. The dose is pre-set at a safe level.
If you have open (laparotomy) surgery you may be offered rectus sheath catheters, which is a continuous infusion of local anaesthetic. This is given via fine catheters (tubes) under the skin alongside your wound.
You will also be given regular paracetamol with the stronger medication, it works differently. Paracetamol seems to work by blocking chemical messengers in the brain that tell us we have pain. It also reduces fever by affecting the chemical messengers in an area of the brain that regulates body temperature.
An opioid is a chemical that works by binding to special opioid receptors in the body (found mostly in the central nervous system and gut), which reduces the pain we feel.
After the epidural or PCA have been removed then you will be offered other effective pain relieving medicines, usually in tablet form. The nurse looking after you will assess your pain level and check the effectiveness of what has been given. Specialist nurses from the Acute Pain Service will visit you regularly if needed.
Tubes and drips
While you are in theatre, a tube (catheter) will be placed into your bladder so that your urine output can be measured. A drain may be inserted into your abdomen to allow any bloody fluid from the operation to be drained away. The urinary catheter is usually removed after 1 to 2 days. If you have an epidural, then your catheter will not be removed until your epidural has been removed.
If you have a drain, this will usually be removed after 2 to 3 days. Depending on the operation your doctor may put other drains in place and they will advise the nursing staff when to remove them.
You will also have a drip put into a vein in your arm. This is so that we can give you fluid to stop you from becoming dehydrated after your operation and to give medication if required. The drip will be stopped as soon as you are drinking enough fluids. The small tube in your vein may stay in for longer if it is being used for medication.
Staying out of bed and walking
Exercises
When you wake up from your operation, it is helpful to start doing deep breathing exercises as soon as possible, repeating them each hour. This will help with your recovery from the anaesthetic.
- Breathe deeply in through your nose, and hold the air in for up to 3 seconds before breathing out through your mouth slowly. You should repeat this 5 times every hour. This will help you to recover from your anaesthetic and prevent a chest infection.
- ‘Huff’ with your mouth open, as if trying to clean your spectacles, this will encourage sputum to clear. If you feel like you need to cough, hold a folded towel over your wound to support your abdomen (stomach) and have one good, strong cough. Repeat this twice every hour.
To help with your circulation while you are lying in the bed or sitting in the chair, you should point your feet up and down and circle your ankles every hour. The therapist will advise you on this technique.
Getting up
The ward staff will help you out of bed as soon as possible after the operation. This may be on the same day. If you are well enough, you should aim to spend 2 hours out of bed the first time out, and then at least 6 hours out of bed the following days (this could be 3 hours in the morning and 3 hours in the afternoon, or 3 sets of 2 hours).
You will be encouraged to walk 20 metres, 3 to 4 times, on the first day after surgery. This will gradually be increased to 60 metres, 4 to 6 times per day, from the second day. (This distance is shown by markers on the corridor wall.)
Being out of bed in a more upright position, and by walking regularly will improve your lung function. It also encourages lots of other body functions where gravity plays a part – for example encouraging normal bowel habits.
Visitors
For visiting times, please visit the Gloucestershire Hospitals NHS Foundation Trust website: www.gloshospitals.nhs.uk
All staff follow a strict confidentiality code. Your treatment/ condition will not be discussed with anyone without your permission. Equally, we are unable to discuss your condition in detail over the phone with anyone, even if they are very close to you.
Discharge criteria and arrangements
You will be discharged from hospital when:
- All of your drips and tubes have been removed.
- You are eating and drinking adequate amounts.
- You are independently mobile.
- Your pain is well controlled.
- Your wound is healing satisfactorily.
- You are passing wind or have passed a bowel motion.
- If you have a stoma formed, you are confident with managing it.
- Any support issues identified have been addressed.
If you feel that you may need extra care after leaving hospital, speak to a member of the nursing or medical staff as soon as possible so that health or social care assessments can be carried out.
Please make arrangements to be collected from the hospital, so that you are ready to go home by 10:00am on your day of discharge.
Important discharge information
Complications do not happen very often, but it is important that you know what to look out for. During the first 2 weeks after surgery, if you are worried about any of the following, please call one of the telephone numbers provided at the end of this page. If you are unable to speak to the people listed then contact your GP for advice.
It is not unusual to suffer gripping pains (colic) during the first week following removal of a portion of the bowel. The pain usually lasts for a few minutes and will go away in between spasms.
Severe pain that lasts for several hours may indicate a leakage of fluid from the area where the bowel has been joined together. This is a rare complication but can be very serious. If this happens you may also have a fever. Occasionally a leak can occur which makes you feel generally unwell, with a fever but without any pain.
If you have severe pain lasting more than 1 to 2 hours or have a fever and feel generally unwell, you should contact us (Colorectal Nurses) on the telephone numbers at the end of this page. Out of normal working hours we would advise you to contact NHS 111 for advice. For emergencies, please call 999.
Your wound
It is not unusual for your wound to be slightly uncomfortable during the first 1 to 2 weeks. If you have either of the following symptoms you should contact your GP for advice.
- Becoming inflamed, swollen or painful.
- Starting to discharge fluid.
Your bowels
Your bowel habits may change after part of your bowel has been removed. Stools may become looser or you may become constipated. This should settle into a more normal pattern over a period of time. If you are constipated, we would advise that you drink plenty of water, take regular walks and increase the fibre intake in your diet (for example, eat more fruit, vegetables, bran and brown bread). If you find you are constipated for more than 3 to 4 days, contact the colorectal team or your GP for advice.
If you are passing loose stools, you should avoid too many foods which are high in fibre, you will need to drink extra liquid to replace the fluid loss. If this does not help, then contact the colorectal team or your GP for advice.
If you have a stoma
On the day of your discharge the stoma nurses will give you a supply of equipment, which you will need, to care for your stoma.
The stoma nurse responsible for your care will discuss any concerns you may have about the care of your stoma when they contact you. This is usually by telephone. The stoma nurse may arrange to visit you at home or to see you in an outpatient’s clinic. You will be given contact telephone numbers and information and advice relating to your stoma before you are discharged from hospital.
On the day of your discharge the stoma nurses will give you a supply of equipment, which you will need, to care for your stoma. The stoma nurse responsible for your care will discuss any concerns you may have about the care of your stoma when they contact you. This is usually by telephone. The stoma nurse may arrange to visit you at home or to see you in an outpatient’s clinic. You will be given contact telephone numbers and information and advice relating to your stoma before you are discharged from hospital.
A balanced, varied diet is recommended and you should try to eat 3 or more times a day. As previously mentioned, you may need to adjust your intake of fibre according to your bowel habits. If you have a stoma, the stoma care nurses will give you specialist advice on your dietary intake.
It is important that you have enough protein and calories to help your body to heal. If you are finding it difficult to eat, you may benefit from supplementing your food with 3 to 4 nutritional drinks a day such as Fortisip® and Fortijuice® which can be prescribed by your GP. Alternatively, Build-up® and Complan® are available to buy in chemists.
If your appetite does not improve after a few weeks, or if you are losing weight without trying, you may benefit from meeting with the dietician. You can ask your consultant, GP or the Colorectal Nurse Specialists to refer you.
Exercise, hobbies and activities
We encourage activity from day 1 following the surgery. You should plan to take regular light exercise several times a day and gradually increase during the 4 weeks following your operation, until you are back to your normal level of activity. Taking up your hobbies as soon as possible again after surgery will also help you to maintain your activity and will benefit your rehabilitation.
The main restriction we would place on exercise or activities is that you do not do heavy lifting until 6 weeks after your surgery. Common sense will guide your exercise and rehabilitation. In general, if your wound is pain-free you can do most activities.
Work
Many people are able to return to work within 4 to 6 weeks after their surgery. If your job involves heavy manual work then we would advise that you take 6 weeks off.
Many people are able to return to work within 4 to 6 weeks after their surgery. If your job involves heavy manual work then we would advise that you take 6 weeks off.
You are likely to feel very tired when you go home, this is normal. Your body needs 2 to 3 months to fully recover from this operation, sometimes longer. It takes time, but you will gradually regain your normal strength.
Remember that you have been through a lot. Some days you may feel tearful, lethargic (tired) and generally have no energy to cope with the things that you feel you should be able to do. This is perfectly normal. You will start to feel well again as your energy levels, strength and fitness returns.
Sex
People often ask when they can have intercourse again after an operation, the answer is ‘when you feel you want to’. The anxiety and all the stress your body has been through with this operation often reduces your sex drive. This is quite normal and in time it will return.
It is important that you and your partner spend time talking about your feelings and being close. This will help both of you to relax more and enjoy your sexual activity when you feel you are ready.
A small number of people can have long term problems due to their surgery. Please talk to your consultant or Colorectal Specialist Nurse if you continue to experience sexual problems.
Driving
Do not drive until you are confident that you can do so safely. It is important that any pain has been resolved enough for you to be able to carry out an emergency stop, to be able to look into your blind spot and turn the wheel quickly with your seat belt on.
We normally advise that you wait for at least 4 to 6 weeks, but if you are unsure then it is best to check with your insurance company before you start driving again.
Questions or concerns
If you have any problems or concerns, or if you have any questions which have not been answered on this page, then please contact the Colorectal Nurse Specialists on the numbers provided at the end of this page.
Hopefully, we will be able to deal with any concerns over the phone, but if you have a problem which requires a physical assessment then we will advise you whether you should come back to see the colorectal team at the hospital, or if you should make an appointment to see your GP.
Contact information
Colorectal Nurse Specialists
Gloucestershire Royal Hospital
Tel: 0300 422 5617
Monday to Friday, 8:00am to 4:00pm
Stoma Care Department
Gloucestershire Royal Hospital
Tel: 0300 422 6702
Monday to Friday: 8:00am to 4:00pm
Cheltenham General Hospital
Tel: 0300 422 4363
Monday to Friday, 8:00am to 4:00pm
Out of hours
(Monday to Friday and weekends)
Telephone the colorectal ward that you were discharged from and ask to speak to the nurse in charge. If the nursing staff are unable to answer your questions, they will contact the on-call doctor for you.
Ward 4A
Gloucestershire Royal Hospital
Tel: 0300 422 6673
Dixton Ward
Cheltenham General Hospital
Tel: 0300 422 3659