Gastroscopy with Radiofrequency Ablation (RFA) for oesophageal dysplasia
You have been offered a treatment to your oesophagus (gullet) called Radio Frequency Ablation (RFA). This page contains information about the treatment and will hopefully answer any questions that you may have. It is important that you read this information so that you understand why you have been recommended for this treatment and what it involves.
On this page
If you are pregnant, taking warfarin, other blood thinning drugs any medication for diabetes, or any drugs to help with weight loss (Ozempic or Mounjaro) please contact the Medication Advice Line as soon as possible for advice. The number is at the end of this page. Your test may be delayed if you do not do so.
Please ensure that you are taking your prescribed proton-pump inhibitor (PPI) medication. If you are not currently taking it, kindly contact us. The number is at the end of this page.
What is dysplasia in the oesophagus?
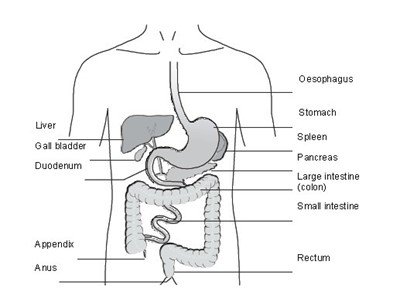
Dysplasia is a term used to describe abnormal microscopic changes in cells lining the oesophagus that have the potential to turn into cancer if not treated.
Dysplasia can be described as Low grade or High Grade and can occur in some patients with Barrett’s Oesophagus and another oesophageal condition called “Squamous Dysplasia”.
To prevent dysplasia potentially developing into Oesophageal cancer, we are able to offer Endoscopy (RFA) treatment which is proven to be effective.
What is the aim of RFA?
Dysplasia and very early oesophageal cancer affects only the cells in the lining layer of the oesophagus.
When we perform the RFA, we can destroy these abnormal cells; once performed we expect the oesophagus lining to heal with normal oesophageal cells. By treating the abnormal cells early and stopping cancer from forming, we hope to avoid more serious treatments like major surgery later on.
Preparing for your procedure
To allow a clear view during the procedure your stomach must be empty. You will be asked not to eat anything for at least 6 hours before your appointment time. You may drink water up to 2 hours before the appointment time.
On admission to the Endoscopy Unit
- You will be seen by a nurse who will check your personal details.
- You will be asked a series of questions about any operations or illnesses that you have had or are currently experiencing.
- Please bring a list of your current medications with you.
- The nurse will want to know if you have any allergies or if you have had any bad reactions to any medications.
- You will be given a drink just before your procedure.
- This drink helps break up saliva and mucous in the oesophagus which allows us to see the area we are treating much more clearly.
- This procedure will be carried out with sedation.
- You will need a responsible adult to take you home when you are ready for discharge.
- You should also have a responsible adult with you at home for 24 hours after your procedure.
- You will also have the opportunity to ask any questions you may have about what is going to happen.
During the procedure
You will be asked to remove any glasses and/or dentures. The monitoring equipment will then be attached. You will be asked to lie on your left-hand side. A plastic tube (known as a cannula) will be placed into a vein in your hand or arm. This will be used to give you the sedative medication. As a safety measure you will be given oxygen via a nasal cannula.
You will then have a local anaesthetic spray applied to the back of your throat to will improve your comfort during the procedure.
- Once you are feeling sleepy, the endoscope is passed down into your oesophagus to look carefully at the area that needs to be treated.
- Once the area has been assessed and we have confirmed that RFA is suitable, we will decide which treatment device is the most appropriate to successfully treat your oesophagus.
- This might be a balloon device which involves us passing a guiding wire will be passed through the endoscope into your stomach. This “guide wire” allows us to accurately position the balloon treatment device in your oesophagus to deliver the RFA treatment.
- Alternatively, if we are treating a smaller area of your oesophagus, we may use a device that we attach to the end of the scope or a device that passes through the scope.
The procedure will take about 30 to 45 minutes, but this will depend on the size of area we are treating.
We will take every measure we can to make sure you are sedated enough for the whole procedure
Complications and risks
RFA has been used to treat patients from all over the world for many years. It has been shown to be a very safe and effective procedure.
As with all endoscopy techniques, there are small risks involved. The major risks can include damage to the oesophagus (perforation) and causing bleeding from the oesophagus. The risk of this happening is about 1 in every 1000 cases.
A small number of patients may develop a stricture or narrowing in the lower oesophagus after RFA treatment. If this happens, an endoscopy will be required to stretch or dilate the area.
After the procedure
After we have completed your procedure, you will be taken, on your trolley, to the recovery area. You will continue to be given oxygen and your blood pressure will be monitored until you are awake.
You should not experience any major discomfort after the procedure but you might be aware of a feeling like heartburn or indigestion.
You will be given a drink when you are awake.
Going home
You will have been given a sedative for the procedure, so you must arrange for someone to take you home. You will also need a responsible adult to stay with you for 24 hours.
For this period, you should not:
- drive a car, motorbike or ride a bicycle
- drink alcohol
- operate machinery or do anything requiring skill or judgement, including cooking
- make important decisions or sign important documents
What can I eat after the procedure?
For the rest of the day following the procedure, you should drink fluids only. Do not drink anything too hot or cold, room temperature is about right.
The day after the procedure, you should start on a soft, sloppy diet and stay on this for a week. This includes breakfast cereals and other food you do not have to chew too much such as mashed potato, minced meat and pasta.
Medication
You should carry on taking your medicine for reducing stomach acid as usual, but for the week after the procedure you should take double your normal amount (dose). You can also take Gaviscon® (this should be
Gaviscon Advanced®) or other antacid liquids, if required. If you experience mild chest discomfort you can take pain relief such as soluble (dissolve in water) paracetamol.
Emergency contact
If you develop any of the following symptoms, you should contact your GP, or if out of normal surgery hours NHS 111 immediately.
- Severe chest pain
- Shortness of breath
- High temperature
- Vomiting or vomiting blood
- Abdominal distension
Follow up
You will receive an appointment in the post to return for another endoscopy to allow us to check that the RFA has been successful. This is usually 2 to 3 months after your procedure. If further treatment is needed, this will be given during this later endoscopy.
Contact information
If you have any questions or concerns about your appointment date or time, please contact the Booking Office.
Booking Office
Tel: 0300 422 6350
Monday to Friday, 8:00am to 4:00pm
Appointment enquiries booking team
Cheltenham General Hospital
Tel: 0300 422 6899
Monday to Friday, 8:30am to 4:00pm
Gloucestershire Royal Hospital
Tel: 0300 422 6351
Monday to Friday, 8:30am to 4:00pm
Medication Advice Line (answer machine)
If you have any questions relating to your medication, please leave a message and a member of staff will return your call:
Cheltenham General Hospital
Tel: 0300 422 3370
Gloucestershire Royal Hospital
Tel: 0300 422 8232
NHS 111
Tel: 111